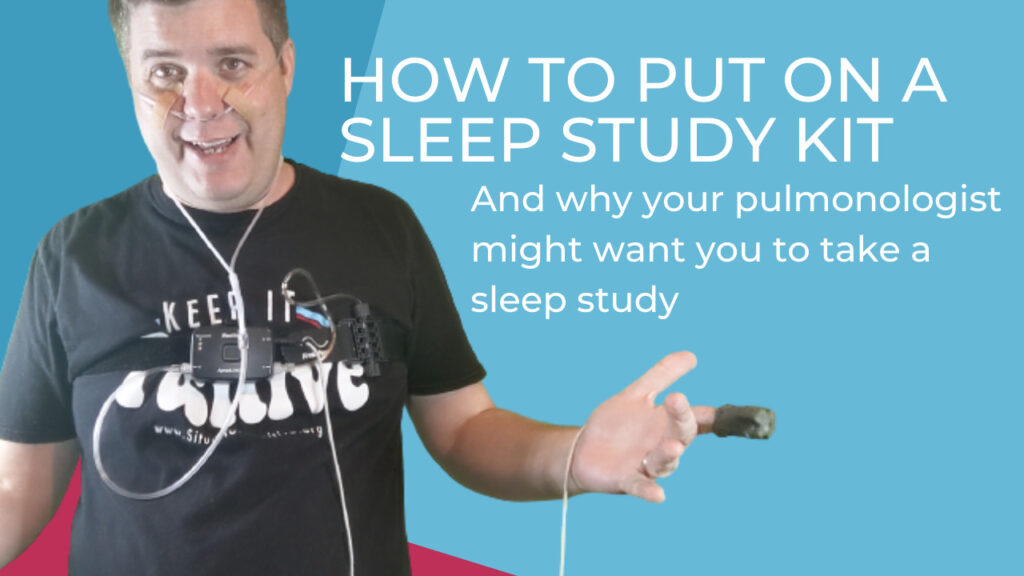
Hey, it is Matt from Situation Positive checking in with you. And it’s about bedtime. And I have to do something interesting tonight. It’s called an at-home sleep study. Did you know that more than 70 million Americans have some kind of sleep disorder? Let me tell you a little bit about mine. So earlier this summer I was having breathing problems.
So I went to see a pulmonologist. A pulmonologist is a doctor who specializes in the respiratory system, the lungs, the windpipe, anything related to breathing. If you’re having breathing issues, you may want to see a pulmonologist. So I went to see my pulmonologist and he treated my breathing issues. And then he wanted to know he was like, Matt, are you having problems sleeping?
And I started thinking to myself, yeah, for years I toss and turn I’m up a couple of times during the night. I can’t tell you the last time I’ve slept through the night without waking up. So he said, Matt, I want to do a sleep study on you. And you know, a sleep study that a pulmonologist is going to do is you’re going to be focused on breathing.
Right? A lot of people have undiagnosed sleep apnea or maybe some other breathing-related sleep disorder. Now sleep apnea. If undiagnosed can end up being fatal, right? So if you’re having problems with sleep, this is something that you should probably look into. So I’m going to try it out right now. I’m going to go ahead and demonstrate how to put on this sleep study kit.
So the doctor gave me this kit. It’s from ResMed. And what you have to do is you get this from the pulmonologist. You take it home, you put it on before you go to bed, you keep it on for at least five hours while you’re sleeping. And then the next day you take it back to the pulmonology office. Okay.
So they can interpret the results. Now, this comes with a bunch of different pieces. It comes with the cannula tube, and this I’m going to insert in my nose. It’s going to track my airflow. Then it also comes with this sensor belt. So this sensor belt I’m going to put around my chest. This serves as an input for all the different tubes.
And it also tracks my movement if I’m rolling around and it’s keeping all of the data that’s happening while I sleep. The last thing is a pulse oximeter, which I’m going to put on my finger and that measures my oxygen saturation. So I’m going to put this all on and hopefully, I can sleep with it on, so let’s go ahead and try it.
So the first thing we got to do is we got to take out the nasal cannula.
So as you can see, it’s just a clear tube. It has these two little, two little things to go in my nostrils. What you want to do is you want to put it over your head behind your ears. And then you can come up.
Is that the way to do it? So I’ve never done this before. So we’re learning together. A few moments later under your chin. Oh, it was under your chin over your ears, and then through your nose. All right. So that took me a little bit to figure out it went under your chin over your ears and then in your nose.
Okay. You know, I’m not a trained professional, so obviously. You know, it took a try or two, and never give up, you know, you gotta do this thing, you gotta do it. Right. So what the, what the nurse recommended and it’s gonna make it even look more silly is to put band-aids on to keep it in place. You don’t want the tube to pop out.
You don’t want to have to do this test again. All right. So here is the second side. We’ll put the band-aid in there. Okay. So next thing I’m going to do is you can loosen this belt. So this belt comes with a
Velcro cord. And you’re just going to slip it over your head and try to get it right around your chest. And then what you want to do is you want to take the Velcro end and once you’ve got it centered on your chest, right about there. You want to pull it so it’s nice and snug. You also then want to a screw in the nasal cannula.
So we’re starting to get there for our sleep study now. And then the final thing we have is to have our pulse oximeter. Okay. You can either put that under your finger or over your finger. Okay. I’m probably gonna put it over my finger because I think as I’ve rolled around at night, this is probably going to be the most comfortable thing for me.
Okay. Once you are all set up like this, you’re ready for bed, right? What could be more comfortable than this? This is why it’s critical to get this stuff, right? Because you only want to have to do this one time. You know, this data is critical to know whether or not you have some sleep disorder related to breathing.
Now, if I do. I’d rather figure that out now. So we can come up with a game plan, my pulmonologist and I, if, if my sleep disorder is related to breathing, let’s go ahead and fix it. And if I have to go through one night of uncomfortable sleep to get those answers, I’m going to do it. Okay. So now that I’m all set, I’m ready to get tucked in and have a good night’s sleep.
When I get done with this in the morning, now I have to keep this on for at least five hours. When I get done with this in the morning I’ll return it to the doctor’s office. They will then take the data that is collected from this machine. And that will go into their overall findings. And I’ll either have a follow-up appointment or a phone call from my pulmonologist.
Where I’ll get the results and we’ll go from there. Okay. So stay tuned. I’ll make sure I post those results. Hopefully, it comes back that I don’t have some kind of sleep apnea, but we’ll see. Thank you so much for tuning in my name’s Matt, this has been Situation Positive, please like, and subscribe for more videos like this, and stay positive everybody!
Podcast: Play in new window | Download (Duration: 9:27 — 17.3MB)